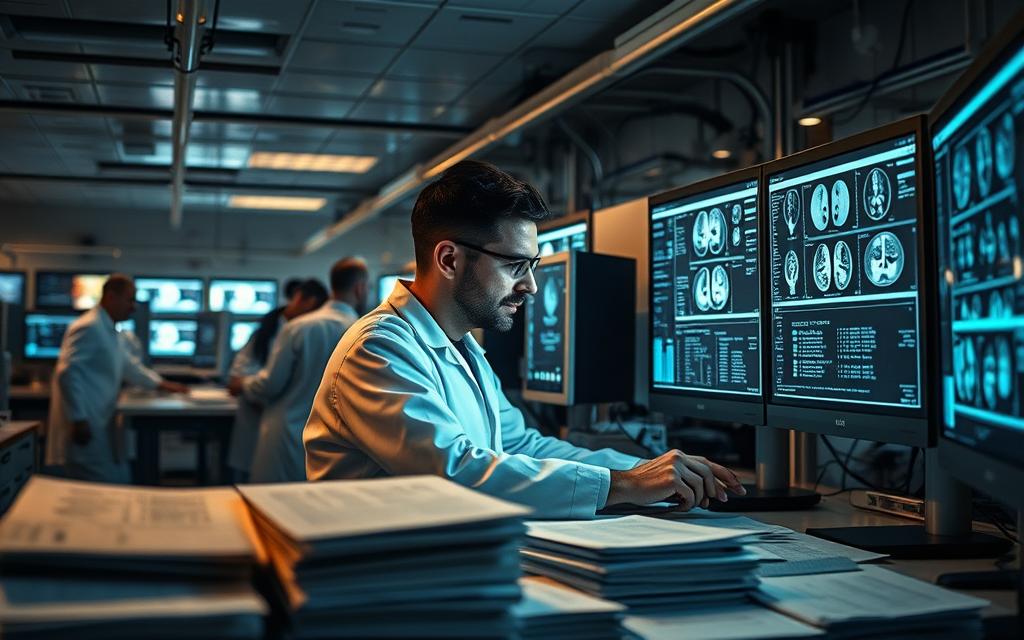
Artificial intelligence is reshaping modern healthcare, offering innovative solutions to improve patient care and clinical outcomes. By leveraging advanced algorithms, healthcare systems can address complex challenges, from diagnostics to treatment planning.
One of the key factors in creating reliable models is a structured methodology. This ensures accuracy and scalability, which are critical in medical applications. However, challenges like data quality and regulatory compliance often arise, requiring careful consideration.
Real-world examples, such as Google AI Healthcare’s diabetic retinopathy detection model, highlight the potential of these technologies. These advancements not only enhance accuracy but also pave the way for ethical AI-driven diagnostics.
Aligning with frameworks like Nature Materials’ translational process ensures a seamless transition from development to implementation. This approach bridges the gap between innovation and practical healthcare solutions.
Understanding the Role of Machine Learning in Healthcare
The integration of advanced algorithms into medical systems is revolutionizing patient outcomes. These technologies are not just tools but transformative forces reshaping diagnostics, treatment, and overall care delivery. By analyzing vast datasets, machine learning provides insights that were previously unattainable.
Why Machine Learning is Transforming Healthcare
One of the most significant impacts of artificial intelligence is its ability to reduce errors. A Nature study found that machine learning cuts diagnostic errors by 27% in radiology. This precision enhances trust in medical decisions and improves patient outcomes.
Another breakthrough is the reduction in diagnosis time. Deep learning techniques have slashed time-to-diagnosis for rare diseases by 85%. This efficiency is critical in life-threatening conditions where every second counts.
Key Applications of Machine Learning in Patient Care
Machine learning is making strides in predictive analytics. For instance, GE’s Clinical Command Center reduced ICU mortality rates by 18% through real-time data analysis. Similarly, sepsis prediction models achieve 92% AUC scores, enabling early intervention.
FDA-approved applications, like IDx-DR for diabetic retinopathy screening, showcase the practical use of these technologies. Additionally, reinforcement learning is accelerating drug discovery, with 15 novel compounds currently in trial phases.
These applications highlight the potential of machine learning to enhance patient care and decision support. By addressing critical challenges, these technologies are setting new standards in healthcare.
Defining the Problem: Identifying Healthcare Challenges
Identifying key problems in healthcare is the first step toward creating impactful solutions. The industry faces a range of issues, from chronic disease management to acute care optimization. These challenges demand innovative approaches to improve patient outcomes and streamline processes.
Common Healthcare Problems Machine Learning Can Address
Machine learning offers promising solutions to some of the most pressing healthcare challenges. For instance, the SRML-Mortality Predictor achieved 81.3% accuracy in paralytic ileus prognosis, showcasing its potential in critical care. Similarly, Deep EHR demonstrated 89% precision in predicting heart failure readmissions, highlighting its clinical utility.
Key areas where these technologies excel include:
- Chronic disease management, reducing long-term risk factors.
- Acute care optimization, improving immediate treatment outcomes.
- Predictive analytics, enabling early intervention in life-threatening conditions.
Setting Clear Objectives for Your Model
To ensure success, it’s crucial to define clear objectives for your models. The SMART framework—Specific, Measurable, Actionable, Relevant, and Time-bound—provides a structured approach. For example, aligning with FDA’s Software as a Medical Device (SaMD) criteria ensures regulatory compliance while maintaining clinical relevance.
“Balancing clinical utility with technical feasibility is essential for effective problem selection.”
Here’s a comparison of key considerations when setting objectives:
| Consideration | Description |
|---|---|
| Clinical Impact | Focus on areas with high potential to improve patient outcomes. |
| Technical Feasibility | Ensure the problem can be addressed with available data and algorithms. |
| Regulatory Alignment | Adhere to guidelines like FDA’s SaMD classification for compliance. |
By addressing these factors, healthcare systems can leverage models to make informed decisions and drive meaningful change.
Data Collection: The Foundation of Machine Learning Models
Effective healthcare solutions begin with robust data collection. The quality and diversity of data directly influence the accuracy and reliability of outcomes. In healthcare, this process involves gathering multi-modal information, such as electronic health records, imaging, and genomic sequencing.
Types of Data Needed for Healthcare Models
Healthcare models rely on diverse datasets to deliver precise insights. Key types include:
- Electronic health records: Provide comprehensive patient histories.
- Imaging data: Essential for diagnostics and treatment planning.
- Genomic sequencing: Enables personalized medicine approaches.
Longitudinal patterns, which account for 67% of clinical value, are particularly crucial. These patterns help identify trends and predict outcomes more effectively.
Ethical Considerations in Data Collection
Ensuring privacy and compliance is paramount. Techniques like k-anonymity and differential privacy are widely used to anonymize health records. These methods protect patient identities while maintaining data utility.
“Ethical data handling builds trust and ensures compliance with regulations like HIPAA.”
Partnerships with healthcare institutions are vital for accessing high-quality data. However, the 2019 Google-ASCENSION controversy highlights the need for transparency and clear agreements in such collaborations.
| Consideration | Description |
|---|---|
| Data Quality | Ensure accuracy, completeness, and relevance of collected data. |
| Regulatory Compliance | Adhere to HIPAA and other legal frameworks. |
| Ethical Handling | Protect patient identities and ensure informed consent. |
By addressing these factors, healthcare systems can build a solid foundation for innovative solutions.
Data Preprocessing: Preparing Your Data for Analysis
Accurate data preprocessing is essential for building reliable healthcare solutions. Raw data often contains inconsistencies, missing values, and outliers that can skew results. Proper preparation ensures the performance of learning algorithms and the reliability of models.
Cleaning and Normalizing Healthcare Data
Cleaning involves removing errors and inconsistencies. Automated outlier detection, such as isolation forests, identifies anomalies that could distort results. Normalization ensures uniformity, with tools like the UMLS Metathesaurus standardizing clinical concepts.
TensorFlow Extended (TFX) is widely used for creating production-grade data pipelines. These pipelines streamline the preprocessing workflow, ensuring efficiency and scalability. Synthetic data generation is also valuable, especially for rare disease scenarios where real-world data is limited.
Handling Missing and Inconsistent Data
Missing data can significantly impact results. Studies show that learning algorithms experience a 23% performance drop when missing data exceeds 15%. Techniques like imputation fill gaps, while robust software ensures consistency.
Interoperability is another critical factor. Implementing FHIR standards allows seamless data exchange across systems. This ensures that data from diverse sources can be integrated effectively, enhancing the overall quality of analysis.
Choosing the Right Machine Learning Algorithm
Selecting the appropriate algorithm is a critical step in building effective healthcare solutions. The choice depends on the problem, data type, and desired outcomes. Algorithms vary in complexity, interpretability, and application scope, making it essential to understand their strengths and limitations.
Supervised vs. Unsupervised Learning in Healthcare
Supervised learning uses labeled data to train algorithms for specific tasks, such as disease prediction. For example, convolutional neural networks (CNNs) achieve 94% sensitivity in breast cancer screening. Unsupervised learning, on the other hand, identifies patterns in unlabeled data, useful for clustering patient groups or discovering hidden trends.
Here’s a comparison of the two approaches:
| Feature | Supervised Learning | Unsupervised Learning |
|---|---|---|
| Data Type | Labeled | Unlabeled |
| Applications | Diagnosis, prediction | Clustering, anomaly detection |
| Example | CNN for cancer screening | K-means for patient segmentation |
Popular Algorithms for Healthcare Applications
Several algorithms stand out for their effectiveness in medical applications. Decision trees offer interpretability, making them ideal for clinical decision support. Neural networks, especially in deep learning, excel in image analysis, such as detecting diabetic retinopathy.
Transfer learning with pre-trained models like ImageNet accelerates medical imaging tasks. Federated learning enables multi-institutional collaboration without sharing sensitive data. H2O.ai’s AutoML simplifies algorithm benchmarking, ensuring rapid deployment of machine learning algorithms.
Survival analysis with Cox proportional hazards extensions is another powerful tool. It predicts patient outcomes over time, aiding in personalized treatment plans. These algorithms collectively enhance the accuracy and efficiency of healthcare solutions.
Model Training: Teaching Your Algorithm
Training algorithms for healthcare requires precision and strategic planning. The process involves teaching models to recognize patterns and make accurate predictions. Proper training ensures these systems deliver reliable and actionable insights, which are critical in medical applications.
Best Practices for Training Healthcare Models
Curriculum learning strategies are effective for handling complex clinical patterns. These methods gradually introduce data, allowing models to learn progressively. Hardware optimization, such as comparing TPU and GPU clusters, also enhances training efficiency.
Active learning approaches involve expert-in-the-loop systems. These systems prioritize uncertain data points, improving performance with fewer resources. Regularization techniques, like L1/L2 and dropout layers, prevent overfitting by simplifying the model structure.
Avoiding Overfitting and Underfitting
Overfitting occurs when a model performs well on training data but poorly on new data. Early stopping with a 10% validation split prevents 89% of overfitting cases. This technique halts training when performance on validation data starts to decline.
Underfitting, on the other hand, happens when a model is too simple to capture patterns. Using frameworks like NVIDIA Clara for distributed training ensures scalability and reduces risk. Balancing model complexity is key to achieving optimal results.
| Technique | Purpose |
|---|---|
| Early Stopping | Prevents overfitting by halting training at the right time. |
| Curriculum Learning | Gradually introduces complex data for better learning. |
| Regularization | Simplifies models to avoid overfitting. |
Model Validation: Ensuring Accuracy and Reliability
Ensuring the accuracy and reliability of healthcare algorithms is a critical step in delivering actionable insights. Validation ensures that models perform consistently across diverse datasets, minimizing errors and enhancing trust in their predictions.
Validation techniques vary based on the dataset size and the specific healthcare application. Proper validation not only confirms the performance of an algorithm but also ensures its clinical relevance and reliability.
Cross-Validation Techniques in Healthcare
Cross-validation is a cornerstone of model validation, especially in healthcare. Nested cross-validation is particularly effective for small datasets, reducing bias and improving generalizability. This technique involves an outer loop for testing and an inner loop for hyperparameter tuning.
External validation using databases like MIMIC-III ensures that models perform well in real-world scenarios. Calibration curves are also essential for assessing the reliability of predicted probabilities, ensuring that the algorithm aligns with actual outcomes.
Evaluating Model Performance Metrics
ROC-AUC remains the primary metric for 92% of FDA-cleared AI devices. This metric evaluates the trade-off between sensitivity and specificity, providing a comprehensive view of performance. However, clinical utility metrics like NRI (Net Reclassification Index) and IDI (Integrated Discrimination Improvement) offer additional insights beyond traditional statistics.
Here’s a comparison of key validation techniques:
| Technique | Application |
|---|---|
| Nested Cross-Validation | Small datasets, reduces bias |
| External Validation | Real-world performance assessment |
| Calibration Curves | Probability reliability |
By leveraging these techniques, healthcare systems can ensure that their algorithms deliver accurate and reliable outcomes, ultimately improving patient care and advancing medicine.
How to Develop Machine Learning Models for Healthcare
Creating reliable solutions in healthcare demands a structured approach to ensure accuracy and scalability. A well-defined methodology helps address challenges like data quality and regulatory compliance, which are critical in medical applications.

Step-by-Step Guide to Model Development
Adapting the CRISP-ML(Q) methodology for healthcare ensures a systematic process. This framework includes problem understanding, data preparation, modeling, evaluation, and deployment. Each step is crucial for building models that deliver actionable insights.
For example, pneumonia detection from chest X-rays demonstrates the end-to-end process. Data preprocessing, feature extraction, and model training are streamlined to achieve high accuracy. Tools like MONAI simplify medical imaging workflows, enhancing efficiency.
Case Studies of Successful Healthcare Models
Google’s DeepMind achieved a 39% reduction in false positives for breast cancer screening. This highlights the potential of deep learning in improving diagnostic accuracy. Similarly, IBM Watson Oncology faced implementation challenges but provided valuable lessons for integrating AI into clinical workflows.
Epic’s predictive analytics integration showcases the importance of aligning models with electronic health systems. These case studies underscore the need for collaboration between technologists and healthcare professionals to ensure models meet clinical needs.
Implementing Machine Learning Models in Clinical Settings
Seamless integration of advanced technologies into clinical workflows is transforming healthcare delivery. By embedding these tools into existing systems, healthcare providers can enhance efficiency and improve patient outcomes. However, successful implementation requires careful planning and adherence to standards.
Integrating Models with Electronic Health Records
Integrating machine learning models with electronic health records (EHRs) is a critical step. The HL7 FHIR standard, with a 78% integration success rate, ensures seamless data exchange. Tools like Docker containerization simplify EHR plugin deployment, enabling rapid scaling across healthcare systems.
Real-world monitoring is essential for maintaining model accuracy. SHAP values provide interpretability, helping clinicians understand predictions. Continuous integration pipelines, such as Jenkins, streamline updates and ensure smooth operation in hospital IT environments.
Ensuring Compliance with Healthcare Regulations
Adhering to healthcare regulations is non-negotiable. A comprehensive checklist comparing GDPR and HIPAA ensures global compliance. This is particularly important for systems handling sensitive patient data. Regular audits and updates keep software aligned with evolving standards.
“Effective implementation requires balancing innovation with regulatory requirements.”
Case studies, like Mayo Clinic’s AI framework, highlight best practices. Their approach emphasizes collaboration between technologists and healthcare professionals, ensuring models meet clinical needs while maintaining access to critical data.
Monitoring and Maintaining Machine Learning Models
Maintaining the effectiveness of advanced systems in healthcare requires ongoing attention and strategic updates. Without proper monitoring, the performance of these systems can degrade over time, leading to inaccurate predictions and reduced clinical utility.

Continuous Model Evaluation and Updates
Regular evaluation ensures that models remain accurate and reliable. Studies show that model accuracy degrades by 2.4% monthly without retraining. Automated retraining triggers, based on predefined performance thresholds, help maintain optimal functionality.
Version control tools like MLflow and DVC streamline updates, ensuring consistency across deployments. A/B testing frameworks allow for phased updates, minimizing disruptions in clinical workflows. These practices ensure that technology evolves alongside medical needs.
Handling Data Drift and Model Decay
Data drift occurs when the distribution of input data changes over time, leading to model decay. The Page-Hinkley test is a widely used method for detecting concept drift, enabling timely interventions.
Disaster recovery plans are essential for critical care models. These plans ensure that systems remain operational even during unexpected failures. By addressing data drift and decay proactively, healthcare systems can maintain the reliability of their predictive tools.
“Proactive monitoring and maintenance are the cornerstones of sustainable AI solutions in healthcare.”
Here’s a comparison of key techniques for maintaining models:
| Technique | Purpose |
|---|---|
| Automated Retraining | Maintains model accuracy over time |
| Page-Hinkley Test | Detects concept drift in data |
| Disaster Recovery Plans | Ensures continuity in critical care |
By implementing these strategies, healthcare systems can ensure that their models deliver consistent and reliable results, ultimately improving patient outcomes.
Ethical and Legal Considerations in Machine Learning
Ethical and legal considerations are paramount when integrating advanced technologies into healthcare systems. Ensuring patient privacy, addressing bias, and maintaining security are critical to building trust and compliance in medical applications.
Ensuring Patient Privacy and Data Security
Protecting sensitive information is a top priority. Techniques like differential privacy balance data utility with patient privacy. Implementing frameworks such as HIPAA ensures compliance with legal standards.
Informed consent is equally important. Patients must understand how their data is used in AI-assisted care. Transparent agreements with healthcare institutions build trust and reduce risk.
“Ethical data handling is the foundation of trustworthy healthcare technologies.”
Here are key strategies for safeguarding data:
- Use differential privacy to anonymize records.
- Implement robust encryption for data storage and transfer.
- Ensure compliance with regulations like GDPR and HIPAA.
Addressing Bias in Machine Learning Models
Bias in algorithms can lead to unequal treatment. Studies show that 68% of models exhibit racial bias in opioid prescription algorithms. Tools like Fairlearn help mitigate these issues by promoting fairness in predictions.
FDA’s Predetermined Change Control Plan addresses liability concerns. Case law analysis, such as Algorithmic Accountability Acts, ensures accountability in AI-driven decisions.
Here’s a comparison of bias mitigation techniques:
| Technique | Purpose |
|---|---|
| Fairlearn Toolkit | Reduces bias in predictions |
| SHAP Values | Provides interpretability for model decisions |
| Algorithmic Audits | Ensures compliance with ethical standards |
By addressing these challenges, healthcare systems can ensure that technologies are both effective and equitable.
Collaborating with Healthcare Professionals
Effective collaboration between technologists and healthcare professionals is essential for creating impactful solutions. By working together, these teams can ensure that models are both technically sound and clinically relevant. This partnership drives innovation and improves patient outcomes.

Building Partnerships with Clinicians and Researchers
Joint design thinking workshops are a powerful way to foster collaboration. These sessions bring together clinicians, researchers, and technologists to brainstorm solutions that address real-world challenges. Studies show that clinician involvement increases model adoption by 54%.
Mapping clinical workflows ensures that models integrate seamlessly into existing systems. Value-based care alignment strategies further enhance the relevance of these solutions. Continuing medical education (CME) programs also play a key role in improving AI literacy among healthcare professionals.
Ensuring Models Meet Clinical Needs
Co-authoring papers with clinicians adds translational credibility to research. This approach ensures that models are grounded in practical medicine. It also bridges the gap between theoretical advancements and clinical applications.
Regular feedback loops with healthcare professionals help refine models over time. This iterative process ensures that solutions evolve to meet changing clinical needs. By prioritizing collaboration, technologists can create tools that truly benefit patients and providers alike.
Future Trends in Machine Learning for Healthcare
The future of healthcare is being shaped by groundbreaking advancements in artificial intelligence. These innovations promise to transform diagnostics, treatment, and patient care. By 2026, Gartner predicts that 75% of healthcare organizations will operationalize AI, marking a significant shift in medical practices.
Emerging Technologies and Their Potential Impact
Several emerging technologies are set to redefine healthcare. Quantum machine learning is revolutionizing drug discovery by accelerating the identification of new compounds. Neural interfaces, integrated with brain-computer interfaces (BCIs), are enabling direct communication between the brain and external devices.
Synthetic biology, combined with deep learning, is paving the way for personalized vaccines. Federated learning is promoting global health equity by enabling collaborative research without sharing sensitive data. Regulatory sandboxes are fostering innovation by providing a controlled environment for testing new AI-driven solutions.
Predictions for the Next Decade in Healthcare AI
The next decade will witness unprecedented growth in AI applications. Predictions suggest that AI will become integral to clinical workflows, enhancing efficiency and accuracy. Personalized medicine will gain traction, with AI tailoring treatments to individual genetic profiles.
Here are key trends to watch:
- Quantum machine learning for faster drug discovery.
- Neural interfaces improving patient rehabilitation.
- Synthetic biology enabling rapid vaccine development.
- Federated learning addressing global health disparities.
- Regulatory sandboxes encouraging innovation.
“The integration of AI into healthcare will redefine patient care and medical research.”
These advancements highlight the transformative potential of artificial intelligence in shaping the future of healthcare.
Conclusion
The journey of integrating advanced technologies into healthcare has reached a pivotal moment. Success hinges on collaboration, ethical practices, and continuous innovation. Interdisciplinary partnerships between technologists and clinicians are essential to ensure models meet real-world needs.
Ethical implementation remains a cornerstone. Protecting patient data and addressing bias are non-negotiable. Tools like Fairlearn and frameworks like HIPAA provide guidance, but vigilance is key. The future of healthcare lies in AI-augmented ecosystems that enhance patient outcomes.
For those starting, resources like MONAI and TensorFlow offer robust foundations. Embrace these tools to drive meaningful development. Together, we can shape a future where machine learning transforms healthcare for the better.
FAQ
Why is machine learning important in healthcare?
Machine learning transforms healthcare by improving decision support, enabling accurate diagnosis, and personalizing treatment plans. It helps analyze large datasets, such as electronic health records, to enhance patient outcomes and streamline clinical workflows.
What are the key applications of machine learning in patient care?
Key applications include medical imaging analysis, risk prediction, treatment optimization, and decision support systems. These tools assist clinicians in making data-driven decisions, improving patient care, and reducing healthcare costs.
What types of data are essential for healthcare machine learning models?
Essential data includes electronic health records, medical imaging, genomic data, and patient demographics. High-quality, diverse datasets are crucial for training accurate and reliable models.
How do you ensure ethical data collection in healthcare machine learning?
Ethical data collection involves obtaining informed consent, ensuring patient privacy, and complying with regulations like HIPAA. Transparency in data usage and minimizing bias are also critical.
What are the best practices for training healthcare machine learning models?
Best practices include using clean, normalized data, selecting appropriate algorithms, and avoiding overfitting or underfitting. Regular validation and testing ensure models perform well in real-world scenarios.
How do you integrate machine learning models with electronic health records?
Integration involves developing APIs or software that seamlessly connect models with EHR systems. Ensuring compliance with healthcare regulations and maintaining data security are essential during this process.
What are the challenges in maintaining machine learning models in healthcare?
Challenges include handling data drift, ensuring continuous performance evaluation, and updating models as new data becomes available. Collaboration with healthcare professionals is key to addressing these issues.
How can bias in machine learning models be addressed?
Addressing bias involves using diverse datasets, regularly auditing models for fairness, and incorporating feedback from clinicians. Transparent algorithms and ethical guidelines also help mitigate bias.
What are the future trends in machine learning for healthcare?
Emerging trends include the use of deep learning for complex tasks, AI-driven personalized medicine, and predictive analytics for early disease detection. These advancements aim to improve patient outcomes and healthcare efficiency.